This 41-Year-Old Dad Thought His Cough Was a Lingering Flu Symptom. It Was Heart Failure

- After months of coughing and having the flu and pneumonia, Son Vang was hospitalized with heart failure.
- Over the course of a few years, his condition worsened, requiring more hospital stays, a heart pump, and placement on the heart transplant list.
- Today, he is thriving and sharing his story to inspire others.
In 2018, 41-year-old Son Vang was living his life as usual. In addition to working and being a father and husband, he spent his free time playing sports, as he had for most of his life.
However, at the end of 2018, Vang came down with pneumonia.
“I had never been quite that sick before,” he told Healthline. “I felt better, and then after pneumonia, I started coughing a lot.”
He eventually recovered, but in the spring of 2019, he got the flu. After taking flu medication, most symptoms subsided, except for a lingering cough.
“My wife was concerned that I kept coughing and couldn’t figure out why,” said Vang. “Two months later, pneumonia happened again, and at this point, we started looking at other things like an x-ray and trying to figure out why I still had fluid and was still coughing.”
Doctors determined that his heart was enlarged and pumping at 25% capacity. He was immediately admitted to the hospital and diagnosed with cardiomyopathy, a type of heart failure in which the heart muscle has difficulty pumping blood throughout the body.
“[The doctors were] surprised I was even walking around looking halfway normal,” said Vang. “I told them I was still working and still doing stuff with my life, but I kind of felt like I was run down all the time.”
Possible causes of cardiomyopathy
Vang’s doctors don’t know the exact cause of his cardiomyopathy. However, Vang believes having pneumonia twice, and the flu may have played a part.
“I even did a genetic test to see if there were issues but there was nothing that showed that,” he said. “But…my heart being damaged a little caused me to get sick, and then it caused me to be sick even worse.”
Sirish Vullaganti, MD, cardiologist at Northwell Health, explained that there are viral infections that can cause cardiomyopathy. When this occurs, it is called myocarditis.
“A virus can actually attack the heart and cause the muscle to become weak, and so that’s certainly possible and goes along with a viral infection that can also affect the lungs, but this is less common than other forms of heart failure,” he told Healthline.
He added that symptoms of cardiomyopathy can also resemble other medical issues, which can lead to misdiagnosis, especially in younger patients who don’t fit the typical profile for heart failure.
For instance, he said this can occur with pneumonia and flu.
“When a patient has a cardiomyopathy, oftentimes fluid can build up in the lungs, and that leads to shortness of breath and a cough, and those are often symptoms that can coincide with a viral infection or a flu,” said Vullaganti. “Sometimes there’s even fever production in heart failure, and sometimes that can be mistaken for indication of other [conditions].”
He has also seen young patients with heart failure misdiagnosed with asthma due to shortness of breath.
“Really, the lungs were fine. It was just their underlying cardiac condition that was leading to their shortness of breath,” he said.
Signs Vang’s condition was worsening after initial treatment
Vang was prescribed medications for heart failure that stabilized his condition. He also changed his diet and lost 20 pounds. Doctors determined that he didn’t need to be on a transplant list.
“[Doctors] figured my heart would recover with the medication, and it did. So, every time I went to see my cardiologist, they tested my blood, and things were better, and I was feeling better to the point where my cardiologist said, ‘I’ll see you next year,’” said Vang.
He carried on for three years until his health took a turn in early 2023.
“I wasn’t feeling well, and I didn’t know why. I lost a little bit of [my] appetite, and I couldn’t eat. I started feeling run down again and I was starting to cough again,” Vang said.
A change in his diuretic caused him to go to the bathroom 15 times in one day. The next day, he had an appointment with his doctor. However, Vang couldn’t remember where he was going or who his wife was.
“I couldn’t answer any of the questions [my wife] asked, and she thought I had a stroke,” said Vang.
The doctor determined that he did not have a stroke but that he was dehydrated from losing too much fluid.
His health continued to worsen, and he ended up in the hospital for three weeks. Doctors informed him that medication was no longer enough to keep him healthy.
“There are many patients who completely normalize their cardiac function with heart failure medication and for the rest of their life have a normalized heart with medication,” said Vullaganti.
However, he said for other patients, their heart failure progresses faster than the medications have time to affect the heart, or the doses can’t be increased enough, or the heart failure is so severe in the beginning that the medications cannot recover the heart function.
“So for those patients we need to think outside the box beyond medications to help them feel better and live longer,” Vullaganti said.

Turning to a heart pump improved his quality of life
For people like Vang who have end stage heart failure, Vullaganti said there are the two options that have been shown to improve life expectancy and quality of life. They can receive a heart pump, known as a left ventricular assist device (LVAD) to help the heart pump blood or a heart transplant.
“Before we designate a patient with that diagnosis, we need to make sure we exhausted all of our options with different medications and devices,” Vullaganti said. “If all of that has failed and patients are still markedly symptomatic and may progress to the point where their heart is not delivering enough blood to the other organs in their body, then we need to think about the LVAD or heart transplant.”
In 2023, Vang’s heart function had become so dire that doctors implanted the Abbott HeartMate 3 LVAD into the center of his chest next to the heart. The device was meant to keep his heart working until he could receive a heart transplant.
“Essentially, an LVAD takes over for a heart that is unable to pump enough blood to meet the body’s demands,” Robert Kormos, MD, divisional vice president of global medical affairs at Abbott, told Healthline.
He explained that the pump takes blood from the heart’s poorly functioning left ventricle and acts as a booster pump to bring blood into the aorta, which bypasses the left ventricle. This allows patients to have more energy and the ability to walk and exercise.
“Additionally, the damage that was done to the patient’s body and other organs over their years with heart failure can be reversed in some instances,” said Kormos.
For people like Vang, the pump can also make him a better candidate for a heart transplant should the time come when he needs it or allow him to live as long as possible without a heart transplant.
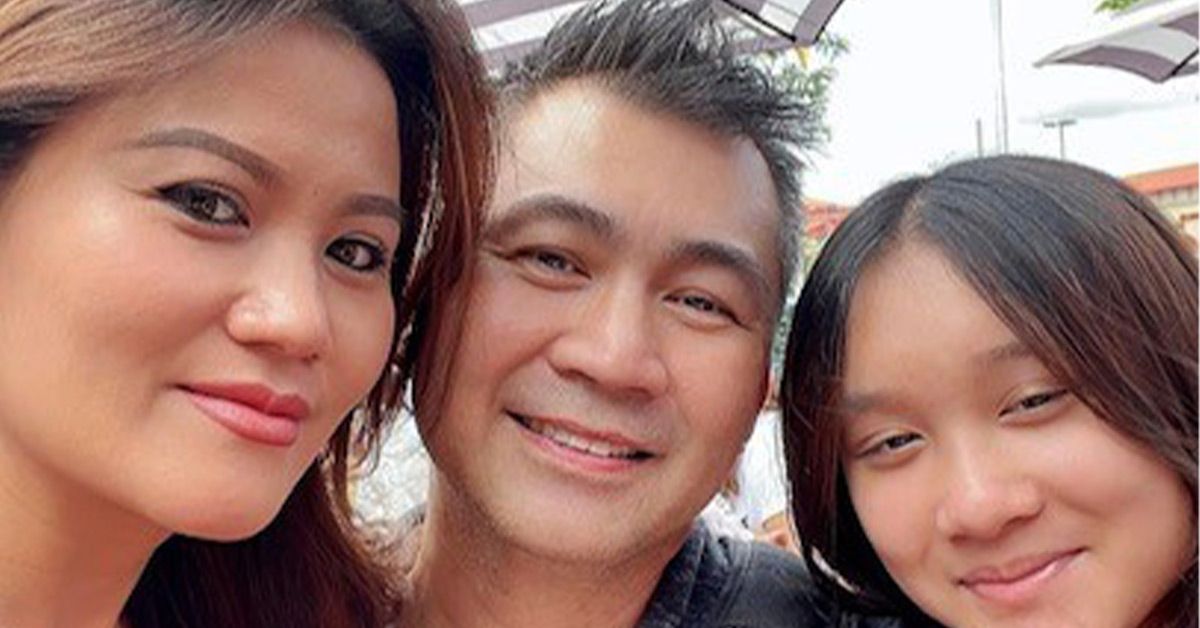
Although Vang received the pump with the intention of having a heart transplant a few weeks later, he has had the pump for over a year and a half. He is back to working, golfing, and enjoying time with his wife and three daughters.
“I’m 47 now, and I feel way better than I did when I was 42 or 43. I’m able to live and enjoy my life a lot better now,” he said.
However, Vang remains on the transplant list in case the pump needs to be removed due to infection or other possible complications.
“This device allows me to stay longer on the transplant list because you don’t want to rush a transplant and have one now and then another one again in 15 years,” said Vang. “[I hope to] extend that by living with [this heart pump] for as long as I can [and push out] the transplant years down the road.”
Source: View source
